UT Arlington-UNTHSC collaboration to build prototype shunt flow monitoring system
July 19, 2015 by PHF Filed under Uncategorized
Scientists from The University of Texas at Arlington and the University of North Texas Health Science Center are building a prototype for an implantable in-line shunt flow monitoring system that would deliver both on-demand and continuous readings of hydrocephalus.
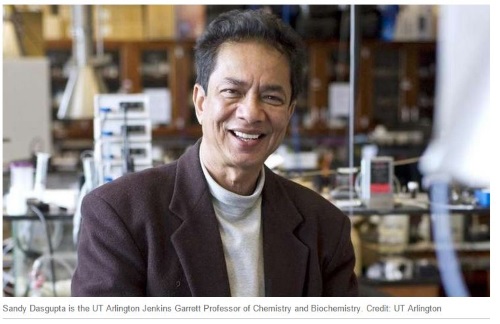
Sandy Dasgupta, the UT Arlington Jenkins Garrett Professor of Chemistry and Biochemistry, and Aditya Das, senior research scientist at the UT Arlington Research Institute, received about $100,000 for the project from the Texas Medical Research Collaborative. The UT Arlington researchers are working closely with Dr. Anthony Lee, a UNT Health Science Center surgeon.
Hydrocephalus is a medical condition in which there is an abnormal accumulation of cerebrospinal fluid in cavities of the brain. This can cause pressure inside the skull which can lead to convulsions, tunnel vision, blindness, balance and coordination issues, mental disability and even death if untreated. Current treatments for the condition utilize a cerebral shunt, or catheter to drain excess fluid. These catheters often can become blocked, infected or outgrown.
The collaborative product could lead to better treatment, especially in infants and children who account for a large proportion of shunt operations every year. About 75,000 shunt operations per year are in infants and children. There is a relatively high rate of complications as late as 17 years after initial placement of the device, according to the National Institutes of Health.
The new shunt system tries to prevent breakdowns by being proactive in monitoring flow of fluids and catheter malfunctions on-demand. It also could help neurosurgeons better understand shunt functions such as whether issues related to malfunction are due to flow or obstruction.
“I have seen the effect of hydrocephalus up close. As a teenager, I saw my infant cousin born with hydrocephalus. He did not survive more than two years,” Dasgupta said. “Now shunt implantation quality of life and life expectancy are far better, but shunt failure and timely diagnosis of that are still problems. It will be a privilege to play a role to help solve this problem.”
Additional benefits of the in-line shunt flow monitoring system include an ability to diagnose in a hospital, outpatient setting or at home in real-time to allow for earlier detection. It also provides research platforms for other biomedical applications including cardiovascular disease treatment and the functional status of artificial organs.
“The entire hydrocephalus community is invested in seeing this research project yield results. Any opportunity to reduce the amount of failures of a shunt, and lengthen the life of the performance of the shunt is welcomed,” said Michael Illions, vice president and director of advocacy for the Pediatric Hydrocephalus Foundation. “A better shunt and less brain surgeries equal a much better outcome for those living with hydrocephalus.”
 Read more at: https://html.com/attributes/img-width/>
Read more at: https://html.com/attributes/img-width/>