Elyse Shares Her Story on Hydrocephalus
March 17, 2016 by PHF
Filed under Uncategorized
Comments Off on Elyse Shares Her Story on Hydrocephalus
Tonight I’m taking you into the life of 6 year old Elyse Clough who’s fighting an incurable brain condition.
Behind Elyse’s smile and long hair are stitches and scars from six brain surgeries. But it doesn’t stop her from being like every other little girl. She loves playing with her big brother Nathan. But some days she can’t play, because she’s sick and her shunt has failed…sending her to get emergency brain surgery.
Her family, along with others, created an organization called REaCH–to research, educate and cure hydrocephalus. This August, the family heads to Washington, D.C to gain support in Congress.
“We try to make money, raise awareness, have a support system for people that have children with Hydrocephalus, we have adults in the group that have Hydrocephalus so it’s been a really good outlet for us to be able to kind of streamline something that’s really bad and make it into something positive and something that has helped a lot of other people,” Kim Clough said.
Tonight at 10 on WFXv and 11 here on WUTR the Clough family shares their in-depth story on Hydrocephalus and Elyse shares her excitement for being a national ambassador.
PHF In The News: Colbert boy raising awareness about hydrocephalus
March 8, 2016 by PHF
Filed under Uncategorized
Comments Off on PHF In The News: Colbert boy raising awareness about hydrocephalus
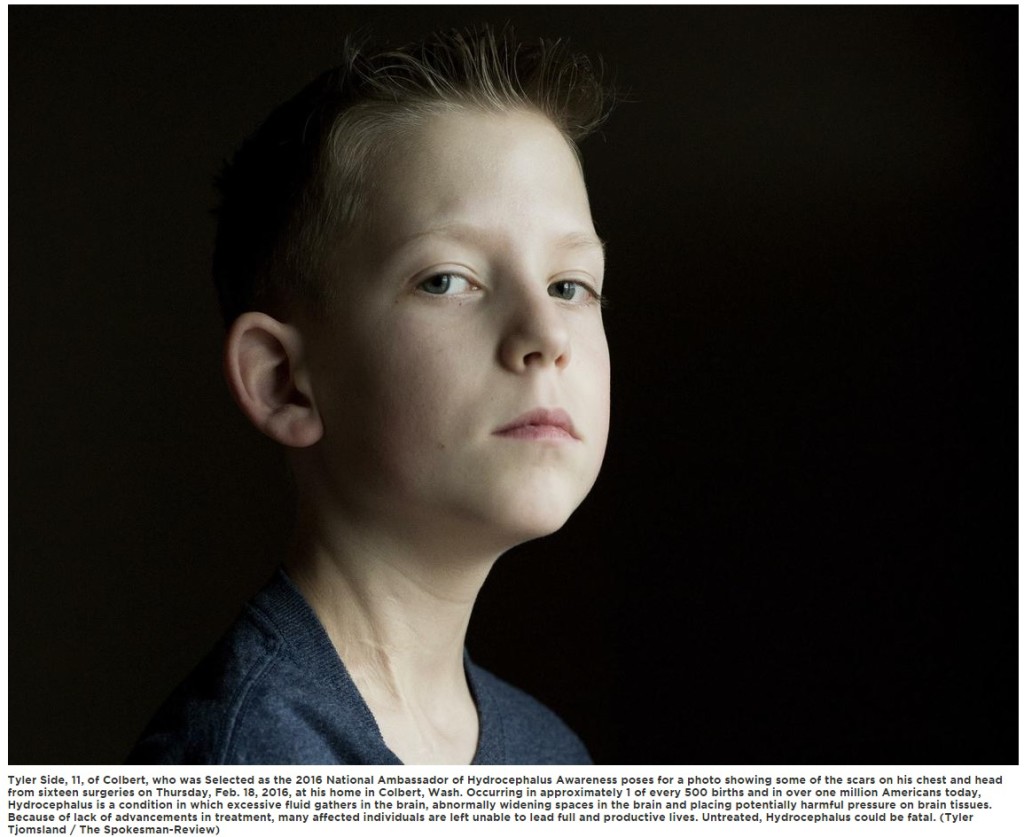
Tyler Side is a cheerful, social boy, who smiles often, but the 11-year-old’s scars reveal a childhood studded with struggle.
Tyler has hydrocephalus, an incurable brain condition characterized by excessive cerebrospinal fluid in the brain’s ventricles, which puts harmful pressure on the tissues of his brain. The scars are from the 16 life-saving surgeries the boy has endured due to the condition.
Now, the Colbert boy will use his story to help others with hydrocephalus. The Pediatric Hydrocephalus Foundation recently selected him as one of two 2016 national ambassadors for pediatric hydrocephalus awareness.
“I feel excited,” he said. “I hope that the hydrocephalus foundation can find a cure for it.”
Tyler will be featured in advertising campaigns and promotional materials heading into the eighth annual National Hydrocephalus Awareness Month in September. He and his family also will travel to Washington, D.C., for National Hydrocephalus Awareness Day on Capitol Hill in August.
So many uncertainties
Tyler was born at just 28 weeks gestation at Ramstein Air Base in Germany, where the Sides were stationed. The pregnancy had been healthy and normal, but placental abruption led to an emergency cesarean section and Tyler was born 11 weeks early, weighing a mere 2 pounds 12 ounces. He was rushed to the neonatal intensive care unit and hooked up to a ventilator.
For many days, doctors didn’t know if he would live. Imaging detected bleeding in his brain.
“It was scary,” said his mother, Crystal Side. “It was very traumatic.”
Despite the news, Side and her husband, Chris, remained hopeful that their baby would pull through, but they were uncertain what that would mean in the long run.
When there was no sign of increased bleeding, the family celebrated, although they learned Tyler might never walk or talk because of the damage.
At 20 days old, doctors diagnosed Tyler with post-hemorrhagic hydrocephalus. The family was flown back to the U.S. by a military medical evacuation flight, still wondering what the diagnosis meant for their family and new baby.
“Would he be able to do the things other kids do? Would he be able to lead a full and productive life? There were just so many uncertainties,” Side said. “It was really difficult as a first-time parent.”
Tyler would go on to have numerous surgeries in his first 10 weeks of life, including a bowel resection following a diagnosis of necrotizing enterocolitis, and the family endured many days in the NICU, hoping Tyler’s progress wouldn’t be set back by more surgeries or infections.
Although he is walking and talking today, Tyler is unable to do many of the physical activities kids his age do because of the condition and the risk of injury. He and his family were ecstatic to learn he was selected to represent the cause – an activity they could give a resounding “yes” to. Side said she hopes her son will see that there are other children like him.
“Having him be able to connect with them will be really special,” she said.
More awareness needed
The causes of hydrocephalus are still not well understood. More awareness is needed, as well as better federal funding for research, said Michael Illinois, vice president and national director of advocacy for the Pediatric Hydrocephalus Foundation.
“Our goal is to provide funding to find better treatment options or help modify or update the current treatment options, while having an eye on one day finding a cure,” he said.
To treat hydrocephalus, a neurosurgeon typically places a shunt system in the body to redirect excessive fluid to other parts of the body, where it is reabsorbed.
Shunts are imperfect systems, and complications – mechanical failure, infections, obstructions, or the need to lengthen or replace the catheter – can result in more surgery, according to the National Institute of Brain Disorders and Stroke.
The condition can be congenital or acquired. Symptoms vary depending on factors such as age and disease progression. In infants, a rapidly increasing skull size is a sign of hydrocephalus, as well as vomiting, sleepiness, irritability and seizures.
The disorder occurs in up to 1 in 500 births and affects 1 million Americans.
Untreated, hydrocephalus can be fatal, and despite medical advances, many with the condition remain unable to lead full and productive lives, according to the foundation.
The all-volunteer nonprofit foundation advocates on behalf of members while working with policy makers at state and federal levels to push for more research and support in the fight against hydrocephalus.
It has 30 state chapters, including in Washington. Since 2010, it has awarded $375,000 in grants and donations to hospital and research centers around the nation.
‘It’s been a long journey’
Despite the challenges he has faced, Tyler has “such a great personality,” his mother said.
“Tyler is such a happy kid and always so pleasant,” she said. “All of his friends, teachers, everyone just loves him.”
She said, “it’s just amazing how well he’s doing.”
“He’s done great,” she said. “It’s been a long journey on some things. To look at him today, most people would never know that he’s been through what he has.”
PHF In The News: Vernon girl gives courage a new face
March 7, 2016 by PHF
Filed under Uncategorized
Comments Off on PHF In The News: Vernon girl gives courage a new face

TOWN OF VERNON — The battle against the brain condition hydrocephalus has found a champion in six-year-old Westmoreland elementary school student Elyse Clough.
Like her namesake (Clough is based on an old Irish word, an Chloch, which means ‘the stone’), Elyse has been a rock for her family through her efforts to live a full life despite her disability.
Her bravery, and her parents’ commitment to help her and others overcome legal and medical barriers to fighting the condition, have led to her being named National Ambassador of Hydrocephalus Awareness for 2016 by the Pediatric Hydrocephalus Foundation (PHF).
“We had formed the group, REaCH, (Research, Educate, and Cure Hydrocephalus) to provide support for those suffering from hydrocephalus and their families and had been in contact with PHF,” Elyse’s mother, Kim, said. “They knew about us and thought Elyse was a good match.”
Later this year Elyse will make a number of appearances on social media and will speak before the U.S. Congress and House of Representatives in Washington, DC on August 19.
Elyse will join her parents and 23 other members of REaCH. Her counterpart, Tyler Side, 11, of Washington State, whom PHF has chosen to represent boys battling hydrocephalus, will join her there. They will stand before the country’s legislative branch to help advocate for continued education and research for her condition.
“It’s been a big deal to her to be chosen,” Kim Clough said.
Her work will continue into September, which PHF has designated as National hydrocephalus Awareness Month for the eighth year.
PHF, which has chapters in 30 states, provides supports to families and also advocates with the medical and legal communities to help find a cure. Since 2010 they have awarded $375,000 in grants and donations towards research and education on the condition.
Hydrocephalus (a combination of the Greek words hydro, or ‘water,’ and kephalos, or ‘head’) is a condition in which an abnormal amount of cerebrospinal fluid accumulates in the brain’s ventricles. The excess fluid causes swelling on the brain.
The ventricles are inter-connected spaces in the brain that produce cerebrospinal fluid; the fluid cushions the brain, helps prevent infection and eases blood flow in the brain.
“The problem is that the fluid will not drain, and there is increased swelling in the brain and other issues,” Elyse’s father, Tom, said.
Hydrocephalus has over 180 different causes. They include birth defects, traumatic brain injury, infection, and overproduction or under absorption of brain fluid. Elyse’s began when she was born premature, at 24 weeks.
“She can be fine one minute and then start having a seizure, and she’s in an ambulance,” Kim Clough said. “Life can change in a minute.”
Along with the risk of seizure, Elyse takes medication for her underdeveloped lungs (caused by her premature birth) and undergoes physical therapy, occupational therapy and speech therapy. She has trouble feeding herself anything besides finger foods. And she’s endured six shunt operations.
Hydrocephalus has no known cure, and the only universally reliable treatment is a shunt implant. (Endoscopic third ventriculostomy, a shunt-free procedure where an incision at the bottom of enlarged ventricles allows fluid to drain only works in two-thirds of patients). A shunt is a soft silicone implant placed in the ventricle, then tunneled under the skin to the abdomen where excess fluid is drained and re-absorbed into the body.
The relief provided by shunts is compromised by their frequent failure rate. Children have a shunt failure rate between 25 and 40 percent. Replacing a shunt is a complicated and potentially dangerous process.
“Every time Elyse, or anyone, has a shunt replaced they require a battery of tests,” Tom Clough said. “They include a CTE scan and several x-rays. Elyse is forced to absorb more radiation than she should have to.”
CTE stands for chronic traumatic encephalopathy, the brain condition recently brought into national attention because of its prevalence among former professional football players.
Elyse is also beginning to deal with the emotional impact of her condition.
“She is becoming more aware of what is happening with her, and she gets nervous sometimes,” Tom Clough said.
Elyse’s state of mind is helped by the presence of her eight-year-old brother, Nathan, who proudly wears a PHF pin on his backpack.
“I’m a sound sleeper, and I missed the ambulance the last time Elyse had a shunt put in (on Feb. 10),” he said. “I stayed with my grandmother the next day, and after I went to school I kept wanting to leave school and check on my sister.”
Nathan’s constant interaction with Elyse has helped her improve her daily living skills.
“She’s very reliant on her brother,” Kim Clough said.
Kim and Tom have joined Elyse in her fight. They formed REaCH in 2010; Kim serves as president and Tom is the group’s treasurer. The group meets once a month at the library in the town of DeWitt near Syracuse.
“It’s important to have the support of those enduring the same challenges that you’re going through,” Kim Clough said.
The Cloughs’ burden is eased by their flexible work schedule. Kim is part-owner of Colonial Pharmacy in Whitestown, where Tom works as an accountant.
“We are able to work around her needs, which is good because she always needs someone with her,” Kim Clough said. “She always comes first.”
Those suffering from hydrocephalus and their families may take solace that the condition, like juvenile diabetes, is not necessarily fatal if properly treated.
“We have all sorts of people of all ages at our meetings,” Kim Clough said. “They won’t let hydrocephalus stop them from living their lives.”
Count Elyse among them. Despite her pain she is planning on living a fulfilling life.
“They asked me in school what I wanted to be when I grow up, and I told them I wanted to be a pediatrician,” she said.
6-Year-Old Elyse Clough From New York Selected as 2016 National Ambassador of Hydrocephalus Awareness for Incurable Brain Condition
February 3, 2016 by PHF
Filed under Uncategorized
Comments Off on 6-Year-Old Elyse Clough From New York Selected as 2016 National Ambassador of Hydrocephalus Awareness for Incurable Brain Condition
6-Year-Old Elyse Clough From New York Selected as 2016 National Ambassador of Hydrocephalus Awareness for Incurable Brain Condition
 Elyse was born on May 26, 2009, 3 ½ months premature, weighing just over a pound. While in the NICU, she had a major brain bleed, which caused her to have fluid accumulation in her brain. After two spinal taps while she was in the hospital, we thought the issue with the excess fluid was resolved.
Elyse was born on May 26, 2009, 3 ½ months premature, weighing just over a pound. While in the NICU, she had a major brain bleed, which caused her to have fluid accumulation in her brain. After two spinal taps while she was in the hospital, we thought the issue with the excess fluid was resolved.
On October 12, 2009, just one month after being discharged from the hospital after birth, Elyse presented with symptoms that we now associate with hydrocephalus. She woke up extremely fussy, vomiting profusely, and when she opened her eyes, only white could be seen. We took her to the pediatrician, who immediately recognized this as hydrocephalus.
We rushed her to the hospital where she had emergency brain surgery to insert her first shunt. This was a terrifying experience. We were unfamiliar with a shunt and with hydrocephalus, and the situation was extremely overwhelming. About three weeks later, we brought Elyse back to the hospital fearing her shunt had failed, since we now recognized the symptoms.
The standard tests that are performed showed no abnormalities, and despite our pleas and efforts, she was released to go home. Later that same week, we rushed her back to the hospital where they determined her shunt had indeed failed. This second shunt failed in June of 2010. After this, Dr. Satish Krishnamurthy, Elyse’s neurosurgeon, along with a group of patients and families struggling with hydrocephalus realized the need for a cure and a support group for hydrocephalus.
That September, REaCH Organization was created. REaCH stands for Research, Educate, and Cure Hydrocephalus. On December 28, 2014, Elyse woke from a nap having a seizure. Again, we rushed her to the hospital, to find that her shunt had failed again. This fourth shunt only lasted until September 5, 2015.
She presented again with a seizure due to the increased pressure in her brain from the excess of spinal fluid. Again, the shunt failed. This shunt revision has been the worst experience for Elyse so far. She unfortunately suffered another brain bleed while the catheter of the shunt was removed, and her recovery has been much slower than before.
It has been very difficult for the entire family. During this recovery, we had a benefit in honor of Elyse to raise money for hydrocephalus research. With the help of many people and businesses, we were able to raise over $10,000 that was given to the Upstate University Hydrocephalus Research Fund.
This money will go directly to Dr. Krishnamurthy’s research to find a better solution and quality of life for those people who suffer with hydrocephalus.
11-Year-Old Tyler Side From Washington State Selected as 2016 National Ambassador of Hydrocephalus Awareness for Incurable Brain Condition
January 31, 2016 by PHF
Filed under Uncategorized
Comments Off on 11-Year-Old Tyler Side From Washington State Selected as 2016 National Ambassador of Hydrocephalus Awareness for Incurable Brain Condition
11-Year-Old Tyler Side From Washington State Selected as 2016
National Ambassador of Hydrocephalus Awareness for Incurable Brain Condition
Up until the night Tyler was born, my pregnancy had gone perfectly and we didn’t have any reason to suspect that the remaining 11.5 weeks would be any different that the first 28.5 weeks had been. At the time, my husband and I were stationed at Ramstein Air Force Base in Germany, away from family and friends, but embracing the culture and travel that being stationed overseas offered. After a day at work and suddenly becoming ill, I agreed to go to the hospital thinking that I would just need fluids to combat what I thought might be the flu. Little did I know that night would change our family’s lives and prove to be one of the most emotional rides we’ve ever been on.
 Tyler was born at 28.5 weeks gestation on January 28, 2005 in Landstuhl, Germany due to placental abruption resulting in an unplanned emergency C-section. At 2 pounds 12 ounces, he was rushed to the NICU to be ventilated and for many days his survival was not certain. Early ultrasounds showed that Tyler had a Grade 2 and Grade 4 intraventricular hemorrhage and we were devastated when the doctor told us that any further evidence of bleeding in his brain would mean that there was nothing else they could do for him. In the days that followed, we were hopeful that Tyler would pull through but uncertain what that would eventually mean.
Tyler was born at 28.5 weeks gestation on January 28, 2005 in Landstuhl, Germany due to placental abruption resulting in an unplanned emergency C-section. At 2 pounds 12 ounces, he was rushed to the NICU to be ventilated and for many days his survival was not certain. Early ultrasounds showed that Tyler had a Grade 2 and Grade 4 intraventricular hemorrhage and we were devastated when the doctor told us that any further evidence of bleeding in his brain would mean that there was nothing else they could do for him. In the days that followed, we were hopeful that Tyler would pull through but uncertain what that would eventually mean.
When there were no additional signs of increased bleeding in his brain, we celebrated but were told that due to the damage, Tyler may never walk or talk, and though the bleeding had stopped, he was not nearly out of the woods. A few days later, at twenty days old, we received news that Tyler had post-hemorrhagic hydrocephalus and at the time had no idea what this meant or how it would affect our precious baby. Since we were still at the military hospital in Germany, we didn’t have access to a pediatric neurosurgeon and were faced with a choice to be transferred to an off-base German hospital or sent back to Bethesda Maryland where he could be treated. We chose the latter and with short notice were moving across the world on a military medical evacuation flight to the National Naval Medical Center. To say that Tyler’s first month of his life was a whirlwind would be an understatement, but we would soon find that the ups and downs had only just begun.
Arriving in Maryland, we were thankful to be stateside, but were still far from our family in Washington State (though we did have quite a few visitors to see our miracle baby!) Tyler’s first shunt was placed externally and it pained us to continue to see him connected to so many tubes, though it did help relieve the pressure which had caused him so much discomfort. Unfortunately, that surgery would be the first of many as Tyler ended up needing a second, third, fourth and fifth external shunt all within 10 weeks. We struggled knowing that the surgeries were necessary but knew that every time the doctors would have to operate, the risk of the shunt failing continued to increase as the white blood cells rushed to heal the site where it could easily clog the catheters meant to help him.
Our next obstacle came when Tyler was diagnosed with necrotizing enterocolitis, and he had to have a large section of his bowel removed. This was another setback in his healing, and we were again filled with questions, worry, and doubt. We often felt so unprepared and spent countless hours and days in the NICU sitting beside Tyler’s bed just hoping and praying that the progress he made each day would not continue to be set back by surgery, infection, and uncertainty.
At just over 3 months in the Bethesda, we were again transferred to another hospital, this time moving to the Children’s Hospital of Philadelphia where Tyler’s shunt would be internalized. While this seemed to be a promising next step, it took a couple tries as the first shunt, a ventricular peritoneal shunt failed due to the scar tissue from the bowel resection. Much to our dismay, the next location that was chosen for Tyler’s shunt placement was through his jugular vein and into his heart, a ventricular atrial shunt.
Nothing seemed scarier, at the time, then knowing that the surgeons were going to feed the catheter through Tyler’s jugular vein toward his heart and have his body absorb the fluid in his bloodstream! Especially in such a tiny body, it seemed impossible that this option would work. However, on May 24, 2005, after nearly 4 months in the NICU, Tyler was finally able to come home!! He had undergone seven shunt surgeries and one bowel resection, but we were elated to finally be leaving the hospital. Being first time parents, we were paranoid about who he was around, if people had washed their hands before holding him, and where he may be exposed to germs, and having him just come home from the hospital after a roller coaster ride his first four months, we were even more paranoid! While the shunt did work for a short time, we did end up in the hospital four more times for shunt revisions in 2005.
Thankfully, however, in 2006, 2007, and 2008, Tyler only needed one revision each year, the last of which was to change the location of his shunt to be a ventricular pleural shunt. During his 2008 surgery, I can clearly remember the pediatric neurosurgeon coming to speak with us after the surgery with a concerned look. The surgery had taken much longer than normal, and the neurosurgeon had described the new location as having to ‘get creative’ in deciding where to go since the many revisions he already had used the most common shunt locations. Thankfully, the new placement was a success and since September 2008, Tyler has only had to have two more revisions, the most recent of which was in July 2014. To date, Tyler’s hydrocephalus has resulted in 16 surgeries so far, and like most parents of a child with hydrocephalus, the next possible shunt failure and surgery is always in the back of your mind.
Anyone that has met Tyler will say he is the sweetest and most charming boy. And any early doubts about his ability to walk or talk were proved wrong as Tyler worked through speech, occupational, and physical therapy to meet major milestones. The resilience and strength Tyler has shown in light of all that he has been through has taught us so much about life and perseverance. At ten (nearly eleven he reminds me), Tyler says he wants to be a doctor when he grows up and he loves riding his bike and scooter, skateboarding, playing video games with his friends, and listening to music.
When I asked him how he feels about having hydrocephalus, he said that sometimes he’s scared and sometimes he is just sad. He’s scared because he doesn’t know when his shunt is going to stop working and it makes him sad that he can’t play soccer like some of the other kids since he can’t get hit in the head. He said, “Being a kid with hydrocephalus is scary because the doctors have to cut into your head to find out what is wrong with your shunt.” But he followed this by saying, “but once, they’re done, then you feel much better.”
We are forever thankful to all of our family, friends, teachers, and medical staff who continue to show such support for Tyler and all he has been through. We are hopeful that with continued research we can improve the technology being used to treat this condition and eventually find a cure!
 Read more at: https://html.com/attributes/img-width/>
Read more at: https://html.com/attributes/img-width/>